Reduce the Growing Cost of Older Adult Falls by Redefining Fall Prevention Care
Why is increasing Fall Rate a problem?
Senior adults’ falls are a common, serious, and rapidly growing public health problem.
As per CDC in 2018,
Falls are also the leading cause of trauma death in any age group.
With the increasing fall rate, a substantial share of healthcare expenditures for adults aged 65 and older is attributable to falls. In 2015, the price tag of direct medical costs to treat non-fatal fall injuries was about $50 billion, fatal injuries was $ 754 million and the average hospital cost for treating fall-related injuries was about $30,000. Of non-fatal fall direct medical treatment costs, 75% of the costs was shouldered by Medicare and Medicaid.
Figure 1: Distribution of Non-Fatal Fall Injury treatment costs
*Direct cost shown above does not include the cost of treating the long-term effects of injuries.
The economic burden from falls is likely to increase substantially in the coming years if more successful fall prevention strategies are not implemented.
Why is the Fall Rate Increasing?
In 2018, adults over 65 accounted for about 16% of the US population, and with more than 10,000 adults turning 65 every day it is expected to increase to 21.6% by 2040. People aged 85+ are the fastest-growing segment of the older population and those at the highest risk for falling.
In the cross-sectional study conducted by the University of Michigan from 2016 to December 2019, of the 120 million Medicare claims analyzed, a 4.4% increase or 1.5% annual growth in fall injury rate was observed. This translates to 106,000 new fall injuries nationally or more than $1 billion in fall injury spending during the study period.
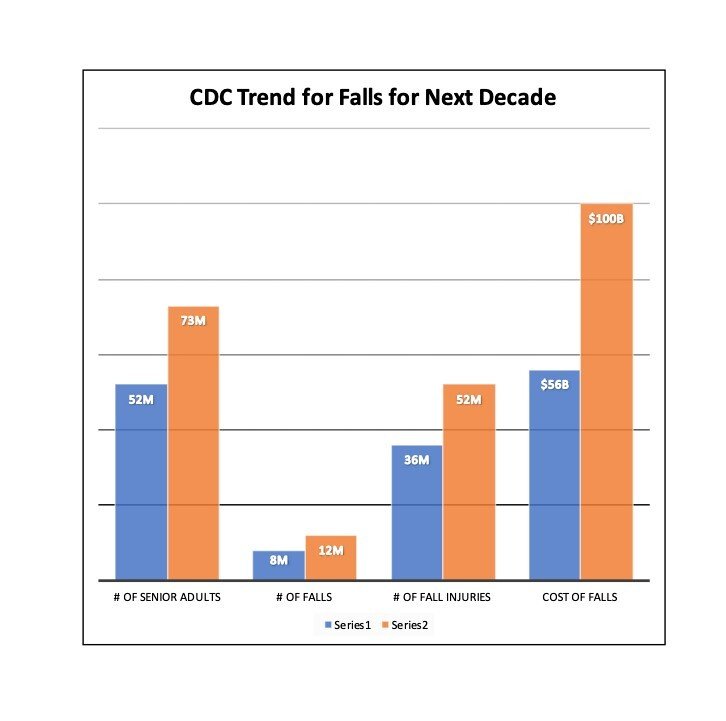
If the fall rate continues to increase at the current pace and based on the projected population in 2030, it is estimated that there will be 5.7 million emergency department-treated falls and 52 million total falls that year and the cost of treating falls is projected to be almost double to $100 billion.
Impact of Covid
In the survey conducted by the University of Michigan since the beginning of COVID-19 pandemic, 46% of older adults reported an increased fear of falling, and one in four adults, who were afraid of falling became more fearful of falling. And 28% of the older adults injured by a fall either delayed or did not receive the medical care they felt they needed.
Why are Falls Getting Worse?
Falling is seen as an inevitable part of the aging process but it is preventable. Research shows screening, multifactorial interventions, and implementing interventions tailored to the patient can reduce falls. Nevertheless, fall risk assessment has not been commonly incorporated into clinical settings. This may be because current practices lack standardization or use complicated methods which rely on either physician expertise, time and/or patient self-reporting.
Although prior fall history has been the best predictor of falls, more than 50% of patients don’t report falls to their physicians. These tools have not been effective in predicting falls: current clinical practices fail to identify 69-85% of patients at risk for falling.
With 21 categories of risk factors for falling, knowing what to do next can be overwhelming if physicians follow typical risk factor identification. It should not be a surprise that 50% of doctors don’t do any screening at all for fall risk.
How Can Falls be Reduced?
Fall prediction can be simplified by looking at the problem differently. Falling is essentially a gravity problem. We should objectively assess the patient’s postural stability – their ability to withstand the force of gravity. Then focus on a simplified set of actionable strategies for intervention and patient empowerment, and retest/monitor regularly for course correction as necessary. These simplified steps with regular measurement can fit into and enhance other chronic condition management, either in clinic or via remote patient monitoring.
Can Tracking Stability Identify Fall Risk and Reduce Falls?
In a 12-month prospective study, 420 older adults had their postural stability measured but were not told their score. They were followed up once a month for detailed conversations with researchers about their balance health and fall incidents. A comparison of the study’s findings with published literature on other standard fall risk screening tools found the new postural stability measurement correctly identified 2-4x more high-risk patients for falling than current clinical practices.
In another prospective study, regular self-testing by older adults in an independent living facility saw a 74% reduction in falls, and the average time to move from high risk to moderate risk was 34 days, indicating that the reduction in falling was the result of measurable improvement in postural stability.
The Technology
Initially developed in the US space program, ZIBRIO’s predictive fall risk assessment is backed by 15 years of research on astronauts, athletes, and older adults. The tool is a specially designed scale that measures postural stability and weight and requires no specialized training, taking just 60 seconds per patient.
Accompanying software guides the clinician through streamlined actionable strategies relevant to each patient, and a patient facing app and education materials can be used to empower the patients. The scale can also be safely used at home as a remote patient monitoring solution to track balance and encourage healthy behaviors.
Better Outcomes Require Better Tools
To combat the rising fall rate and fall treatment costs of an increasingly elderly population, providers and payors will need to prioritize objective, accurate screening for every older adult, and couple that with streamlined actionable strategies available in the community that the physician can prescribe or refer: e.g., physical therapy, Tai Chi, Otago, A Matter of Balance. The successful strategies will be those paired correctly with the patient’s level of ability and motivation and may be coupled with appropriate medications review.
Regular follow-up measurement should be included as part of routine care and incorporated into remote patient monitoring where appropriate for certain segments of the population.
Physicians need robust tools that fit into current workflows in order to make meaningful changes in the falls epidemic we’re entering. After all, a fall makes managing the rest of patient’s health issues more complex and expensive. And effective fall prevention modalities, like exercise, often have a positive impact on chronic condition management.
To learn more about ZIBRIO technology click here or Schedule a 20 minute personal Zoom demo and get all your questions answered.